Description
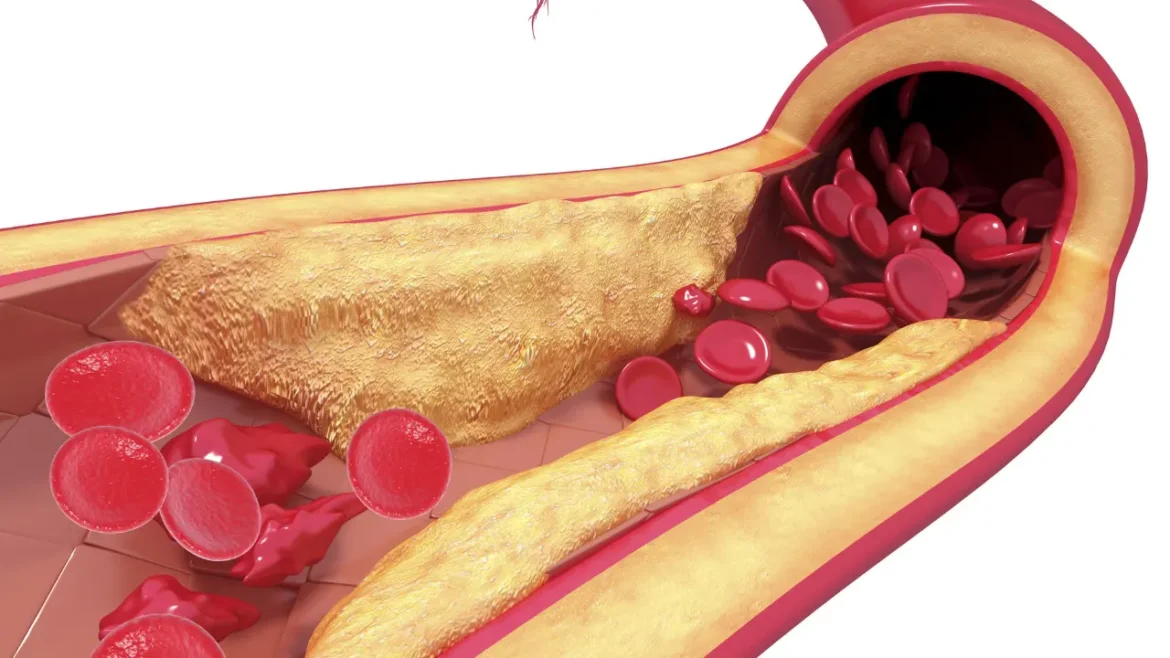
A rare disorder known as autoimmune hyperlipidemia is marked by a disruption of lipid metabolism as a consequence of an autoimmune reaction that targets lipoproteins. The aberrant lipid levels caused by this immune-mediated malfunction include higher levels of triglycerides and low-density lipoprotein cholesterol (LDL-C). Owing to the condition’s complicated origins and specific problems, treatment must take a diverse approach. A number of distinct diseases fall under the umbrella term of autoimmune hyperlipidemia, comprising autoimmune mixed hyperlipidemia, autoimmune mixed dysbetalipoproteinemia, and autoimmune hypercholesterolemia. Different lipid abnormalities and related clinical symptoms define these illnesses. Lipemia retinalis, xanthomas, and persistent stomach discomfort are among the symptoms that people with autoimmune hyperlipidemia frequently display.
You May Also Like:
TOP 3 MUSHROOMS FOR MEMORY– YOU WILL NEVER FORGET NUMBER ONE
THE CONNECTION BETWEEN MUSHROOMS AND COVID: 5 GREAT REASONS TO TRY FUNCTIONAL MUSHROOMS
Autoimmune Hyperlipidemia: Description, Causes, and Treatment Protocol is an original (HealthXWire) article.
Possible Causes
Uncertainty surrounds the precise etiology of autoimmune hyperlipidemia. The illness is thought to be influenced by both environmental and hereditary factors, though. The following are some potential reasons and contributing factors: –
Autoimmune Dysfunction: An autoimmune reaction that targets lipoproteins, particularly LDL cholesterol (LDL-C), is what defines autoimmune hyperlipidemia. Autoantibodies are created by the immune system against lipoproteins because it incorrectly thinks they are foreign molecules. A dysregulated lipid metabolism and aberrant lipid levels may result from this immunological response.
Genetic Factors: Some data that suggests genetic predisposition contributes to autoimmune hyperlipidemia. Immune system control, lipid metabolism, and the emergence of autoimmune responses may all be impacted by certain genetic variants. Autoimmune hyperlipidemia can be seen to cluster in families, pointing to a hereditary element.
Other Autoimmune Diseases: Autoimmune disorders like rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and autoimmune hyperlipidemia frequently coexist. Such underlying autoimmune disorders’ existence raises the possibility of a common immunological mechanism driving the emergence of autoimmune hyperlipidemia.
Environmental Factors: The onset and course of autoimmune hyperlipidemia may be influenced by environmental variables like nutrition and lifestyle. A high-fat diet can cause dyslipidemia and raise the possibility of autoimmune hyperlipidemia, especially if it is heavy in saturated and trans fats. Smoking, obesity, and a sedentary lifestyle are all contributors to lipid abnormalities and might make the problem worse.
Medical Conditions and Medication: Autoimmune hyperlipidemia may develop or worsen as a result of specific drugs and health issues. Medications like corticosteroids, oral contraceptives, immunosuppressive treatments, and antiretroviral therapies have been linked to lipid abnormalities. Furthermore, medical disorders, including hypothyroidism, and chronic renal disease, might affect lipid metabolism and raise the probability of dyslipidemia.
Hormonal Factors: Hormonal changes may influence lipid metabolism and contribute to autoimmune hyperlipidemia. As an illustration, hormonal imbalances brought on by illnesses like polycystic ovary syndrome (PCOS) or menopause can cause dyslipidemia and raise the likelihood of lipid abnormalities.
Exacerbating and Mitigating Factors
Exacerbating Factors: –
Obesity: Elevated LDL-C levels and decreased HDL-C levels are linked to excess body weight, especially abdominal obesity. Additionally, aggravating lipid problems are obesity’s role in insulin resistance along with metabolic disorders.
High-Fat Diet: A diet rich in saturated and trans fats may increase triglyceride and LDL cholesterol or LDL-C levels, aggravating abnormalities in lipids in autoimmune hyperlipidemia.
Sedentary Lifestyle: Lipid metabolism can suffer from a lack of consistent exercise. Reduced triglyceride clearance and reduced HDL-C levels are linked to physical inactivity and dyslipidemia, respectively.
Underlying Autoimmune Diseases: Systemic lupus erythematosus, rheumatoid arthritis, and autoimmunity hyperlipidemia are autoimmune disorders that frequently co-occur. It is possible that the disruption of lipid metabolism in these circumstances is a result of the underlying autoimmune disease.
Certain Medications: In autoimmune hyperlipidemia, several drugs might worsen lipid abnormalities. Examples include oral contraceptives, immunosuppressive treatments, corticosteroids, and some antiretroviral therapies.
Mitigating Factors: –
Regular Exercise: Consistent physical activity has many advantages for lipid metabolism. HDL-C levels can be increased and lipid profiles can be improved by aerobic sports like cycling or brisk walking. Exercises that involve strength may help lipid metabolism.
Healthy Diet: In autoimmune hyperlipidemia, lipid profiles might be improved by switching to a heart-healthy meal reduced in cholesterol, trans fats, and saturated fats. Place a strong emphasis on eating a variety of vegetables, fruits, whole grains, lean meats, and healthy fats such as people in seeds, nuts, and fatty fish.
Weight Management: Maintaining a healthy weight through a combination of nutrition and physical activity can help with lipid problems. Losing weight can raise triglyceride levels and decrease LDL-C levels in overweight or obese individuals.
Smoking Cessation: To control autoimmune hyperlipidemia, smoking must be stopped. Smoking impacts lipid metabolism, causing elevated LDL-C and decreased HDL-C levels. Smoking also destroys blood arteries.
Limiting Alcohol Consumption: Overindulging in alcohol can increase triglyceride levels and cause liver damage. To lessen lipid abnormalities, alcohol should be consumed in moderation or not at all.
Medication Review: Several drugs may make lipid problems worse. To determine any potential effects on lipid profiles, it is crucial to discuss all drugs with a healthcare provider. If necessary, adjustments or different medications might be thought about.
Stress Management: Lipid metabolism may be negatively impacted by long-term stress. Participating in stress-relieving exercises, like yoga, meditation, or hobbies, can lessen the effect of stress on aberrant cholesterol levels.

Standard Treatment Protocol
The typical course of treatment for autoimmune hyperlipidemia combines medicine with changes in lifestyle. Reduced levels of LDL cholesterol (LDL-C), normalized triglyceride levels, and decreased risk of cardiovascular problems are the main targets of treatment. The following is the recommended course of treatment for autoimmune hyperlipidemia: –
Lifestyle Modifications: These include: –
- Weight Management
It is essential to reach and keep an ideal body weight. Losing weight can lower LDL-C levels and boost triglyceride levels.
- Diet
A diet that is reduced in saturated and trans fats is advised. Consuming an assortment of whole grains, vegetables, fruits, and lean proteins falls under this category. Aside from that, consuming less cholesterol is also crucial.
- Exercise
Regular exercise, particularly aerobic exercise, and training for strength, can help to enhance lipid profiles and cardiovascular health in general. Aim for 150 minutes or more of moderate-intensity exercise each week.
- Alcohol Moderation
It is advised to limit alcohol use because excessive alcohol use can increase triglyceride levels.
- Smoking Cessation
Smoking has negative impacts on cardiovascular health and lipid metabolism.
Pharmacotherapy: These include: –
- Bile Acid Sequestrants
These substances, like cholestyramine, adhere to bile acids within the colon, blocking enterohepatic circulation and increasing LDL receptor activation, and decreasing LDL-C levels.
- Statins
The cornerstone of pharmaceutical therapy for autoimmune hyperlipidemia is statins. By preventing the liver from producing new cholesterol, they successfully reduce LDL-C levels. Atorvastatin and rosuvastatin are two examples of statins.
- Fibrates
When it comes to decreasing triglyceride levels and raising HDL cholesterol (HDL-C) levels, fibrates like fenofibrate are very beneficial.
- PCSK9 Inhibitors
Inhibitors of proprotein convertase subtilisin/kexin type 9 (PCSK9), like alirocumab and evolocumab, are more recent drugs that can be used to treat people who suffer from inherited hypercholesterolemia or refractory hyperlipidemia.
- Cholesterol Absorption Inhibitors
Ezetimibe provides an illustration of a cholesterol-absorbing inhibitor that suppresses LDL-C levels by preventing the absorption of cholesterol through the diet.


Treatment Options
The efficacy of conventional treatments can be increased by considering adjunct therapies along with the regular treatment plan. To maintain safety and prevent any interactions, patients must speak with a healthcare provider before beginning any adjunct therapies. Following are some possible therapies: –
Over-the-Counter Formulations: These include: –
- Omega-3 Fatty Acids
Fish oil supplements frequently contain omega-3 fatty acids, which have been demonstrated to reduce triglyceride levels. They could be a supplement to medication.
- Stanols and Plant Sterols
By lessening cholesterol absorption within the intestine, these substances, which are sold available in the form of over-the-counter supplements, may assist in lowering LDL-C levels.
Nutritional Supplements: These include: –
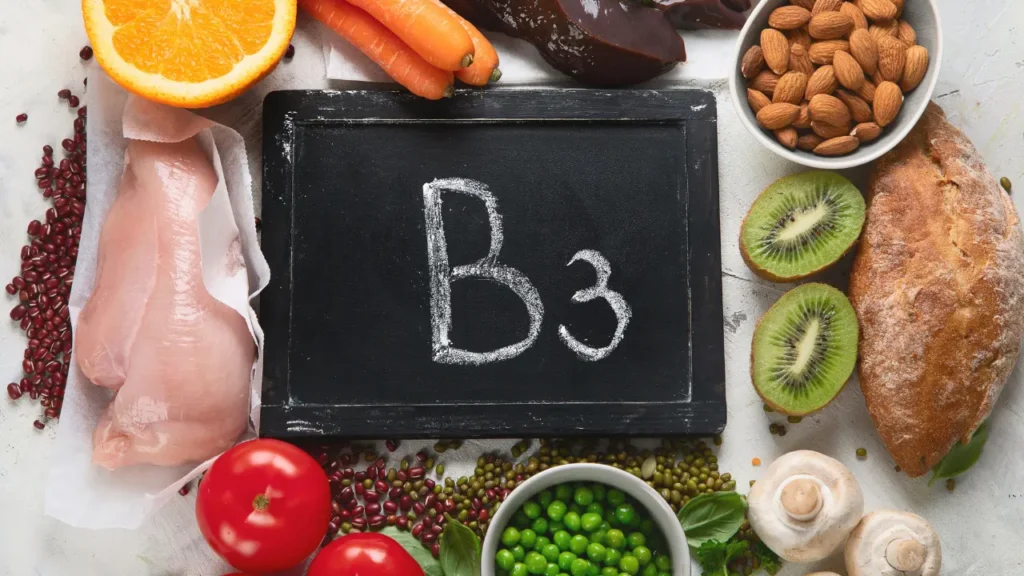
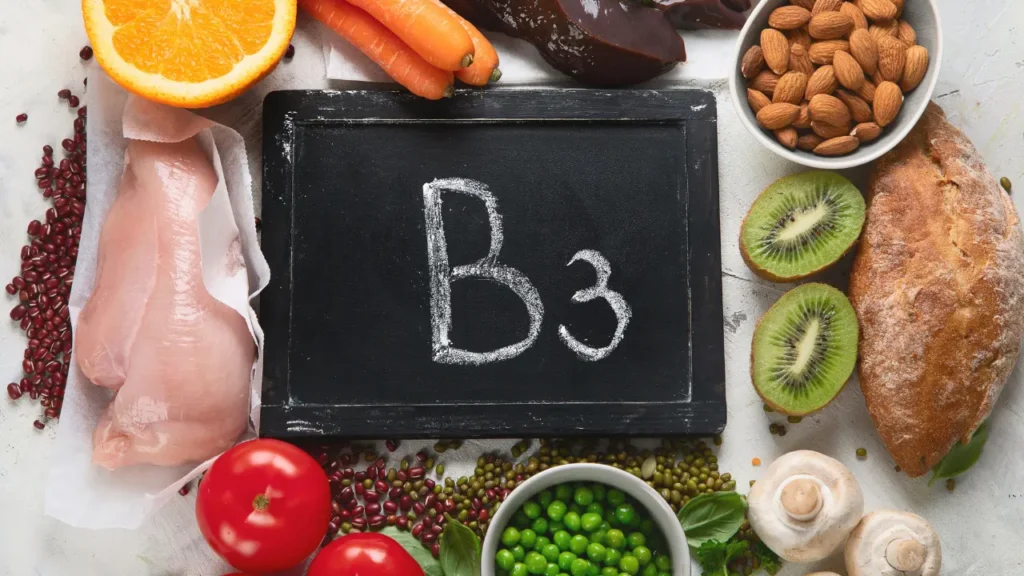
- Niacin
A B vitamin called niacin can help increase HDL levels while reducing triglyceride and LDL levels. Due to probable negative effects, it ought only to be utilized under the supervision of a medical practitioner.
- Soluble Fiber
Soluble fiber might be added to the diet either naturally or through supplements, which can lower LDL-C levels.
Natural and Herbal Remedies: These include: –
- Green Tea Extract
Polyphenols included in green tea extract can impose a minor impact on lipid profiles. It might be utilized as an addition to conventional care but shouldn’t take the place of it.
- Garlic
Supplements containing garlic could provide some anti-inflammatory benefits and have been linked to moderate drops in LDL-C levels. But because there is not enough research to support it. Hence, it is inappropriate to use it in place of prescription drugs.
- Red Yeast Rice
Statins, like lovastatin, which are present in red yeast rice naturally can reduce LDL-C levels. Red yeast rice may differ in potency. Thus, it should be utilized cautiously as it might interact with drugs.
Nevertheless, it is crucial to remember that, even though adjunct therapies might provide advantages, they should not be utilized in place of regular medical care. Before including any adjunct medicines in their treatment plan, patients should always speak with a healthcare provider to explore their appropriateness, assurance, and potential interactions.
Conclusion
Autoimmune hyperlipidemia occurs when the disruption of a bodily metabolism that regulates lipids. The disruption is complicated and can lead to chronic consequences such as elevated cholesterol and triglyceride levels which also increase the risk of cardiovascular diseases. Hence, early detection and prompt management are essential. A diverse approach must be taken to treat autoimmune hyperlipidemia since it is complex and can stem from multiple origins. It can stem from autoimmune dysfunction, genetic predisposition, and also environmental factors.
A combination of lifestyle modifications, standard treatment protocol, and nutritional support will be a good plan to treat patients with autoimmune hyperlipidemia. A standard protocol includes regular monitoring of lipid profiles, weight management, diet, and others. By implementing a comprehensive treatment plan and promoting patient adherence, healthcare providers can mitigate the impact of autoimmune hyperlipidemia on patients’ health, ultimately reducing the burden of cardiovascular complications associated with this complex autoimmune disorder.
Additional resources for further reference
https://pubmed.ncbi.nlm.nih.gov/168771/
https://www.amjmed.com/article/0002-9343(75)90355-1/fulltext
https://www.baptisthealth.com/care-services/conditions-treatments/hyperlipidemia
https://my.clevelandclinic.org/health/diseases/21656-hyperlipidemia
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.
Table of Contents