Description
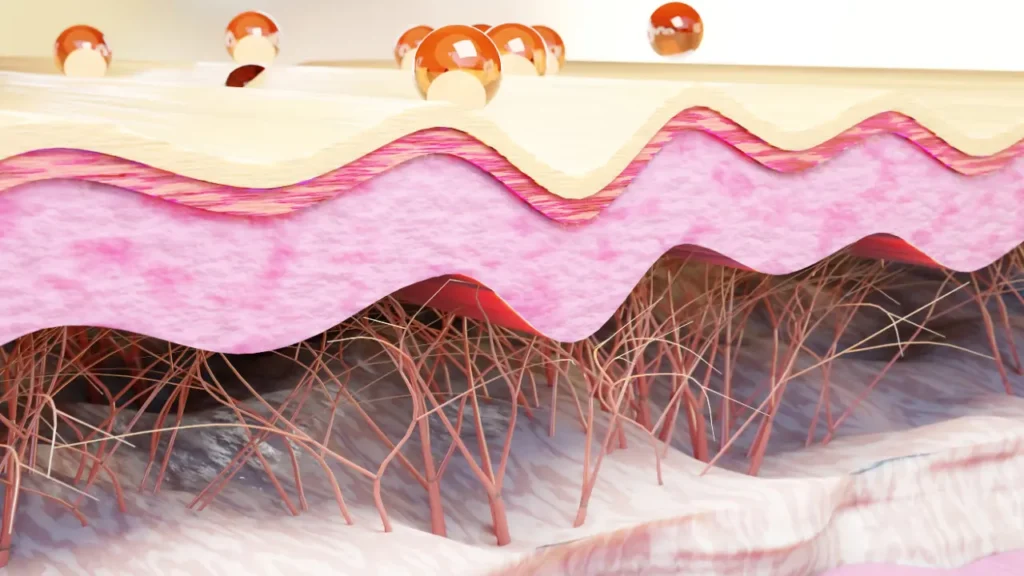
Scleroderma is a rare autoimmune condition that causes the connective and skin tissues to tighten and harden. A variety of symptoms and problems can result from the disease’s potential impact on numerous organ systems. If you have been diagnosed with this condition, thorough care requires an understanding of the causes and available treatments. Scleroderma is divided into two primary categories: systemic sclerosis, which impacts the internal organs and skin, and localized scleroderma, which mostly affects the skin.
The increasing fibrosis of the internal organs and skin, including the lungs, kidneys, heart, and gastrointestinal system, is the defining characteristic of systemic sclerosis. The condition can also show up as Raynaud’s phenomenon, which is what causes the thickness of the skin, stiffness of the joints, or organ malfunction.
You May Also Like:
HOO RAA CBD VS PARTNERED PROCESS CBD
SKIN BIOPSY: DESCRIPTION, CAUSES, AND TREATMENT PROTOCOL
Scleroderma: Description, Causes, And Treatment Protocol is an original (HealthXWire) article.
Possible Causes
Researchers think that a mix of immune system, environmental, and genetic variables have a role in the development of scleroderma, while the exact causes are not entirely understood. The following potential causes have all been looked at:
Autoimmune Dysfunction: As an autoimmune illness, scleroderma is characterized by an aberrant immune response in which the body’s defenses wrongly target healthy tissues. The immune system seems to become dysregulated in those with scleroderma, resulting in excessive collagen formation and inflammation. Uncertainty persists over the precise causes of this immunological condition.
Genetic Factors: Existing data suggests some genetic differences may increase scleroderma susceptibility. Studies have uncovered certain genes linked to collagen formation and immune system modulation that may contribute to the disease’s onset. Scleroderma cannot, however, be caused solely by genetic reasons; other variables are certainly also at play.
Environmental Triggers: Scleroderma may be brought on by environmental factors including viral infections or exposures to specific toxins. Studies have revealed a link between the onset of the illness and specific viruses like the Epstein-Barr virus. Scleroderma risk may also be increased in some people if they are exposed to chemical solvents or silica.
Vascular Abnormalities: Vascular abnormalities such as tiny blood vessel destruction and reduced blood flow are hallmarks of scleroderma. Although the precise mechanisms are still unclear, medical researchers believe that these vascular alterations contribute to the inflammatory and fibrotic processes found in scleroderma.
Exacerbating and Mitigating Factors
Scleroderma management heavily relies on exacerbating and alleviating factors. Finding these factors can assist those with scleroderma in making lifestyle changes and adopting tactics to reduce symptom flare-ups while improving general well-being. The following are some typical scleroderma aggravating and mitigating factors:
Emotional Stress: Scleroderma sufferers can experience symptom flare-ups as a result of anxiety, stress, and emotional turmoil. Stress can be managed with mindfulness exercises, therapy, support groups, and relaxation methods.
Cold Temperatures: Raynaud’s phenomenon, a prevalent scleroderma symptom marked by aberrant blood vessel spasms in reaction to cold or stress, can be brought on by or aggravated by being exposed to cold temperatures. By using hand warmers, dressing in layers, and staying warm, you can reduce discomfort.
Certain Medications: Some drugs, including beta-blockers and specific chemotherapeutic drugs, might worsen symptoms or induce unpleasant reactions if you have been diagnosed with scleroderma. Before beginning any new medications, it is critical to let your doctor know you have scleroderma.
Smoking: Smoking is believed to aggravate scleroderma symptoms and quicken the disease’s progression. Giving up smoking is essential for good health and can greatly improve outcomes if you already have the disease.
Infections: Infections like urinary tract or respiratory infections cantrigger symptoms in those with scleroderma or make them worse. Maintaining excellent hygiene habits, receiving required vaccinations, and quickly treating infections can all help lessen their effects.
Mitigating Factors:
Healthy Lifestyle: Scleroderma management can benefit from maintaining a healthy lifestyle. This involves staying active regularly, eating a balanced diet full of vegetables, fruits, and whole grains, along with abstaining from binge drinking.
Environmental Triggers: Scleroderma sufferers can lessen their symptom exacerbation by identifying and preventing environmental triggers like exposure to organic solvents, silica, or particular chemicals.
Consistent Monitoring and Follow-Up: Scleroderma specialists can help track the development of the condition, spot any complications early on, and modify treatment regimens as necessary with periodic follow-up visits.
Patient Support and Education: Awareness of the condition, how to manage it, and the tools that are accessible can enable those with scleroderma to take control in their treatment. Support networks and advocacy groups offer important assistance, knowledge, and chances to connect with others going through similar struggles.
Skin Care: The management of scleroderma-related skin problems requires proper skin care. This means regularly moisturizing, preventing harsh chemicals, shielding the skin from overexposure to sunlight, and using mild cleansers.


Standard Treatment Protocol
Scleroderma is typically treated with a multidisciplinary strategy to address the various disease symptoms. The typical treatment protocol’s key elements are listed below:
Medications:
- Corticosteroids
Prednisone and other corticosteroids can help reduce inflammation and treat symptoms, but prolonged usage is generally discouraged because of the potential negative effects.
- Immunosuppressants
Medications like mycophenolate mofetil, methotrexate, and azathioprine can be administered to suppress the body’s immune response and minimize inflammation.
- Proton Pump Inhibitors (PPIs)
In order to treat gastroesophageal reflux disease (GERD), a condition that is frequent in people with scleroderma, PPIs like pantoprazole or omeprazole can help in reducing symptoms.
- Vasodilators
By increasing blood flow and decreasing vascular constriction, calcium channel blockers such as nifedipine or ACE inhibitors like captopril can be used to treat Raynaud’s phenomenon.
Symptomatic Management:
- Physical therapy
Maintaining joint flexibility, reducing muscle stiffness, and enhancing general function can all be achieved with the help of physical therapy, which includes range-of-motion movements and exercises.
- Pain relief
To treat stiff joints and pain, nonsteroidal anti-inflammatory medications or NSAIDs like acetaminophen or ibuprofen can be taken.
- Topical treatments
To control skin problems and lessen dryness and irritation, doctors may prescribe moisturizers, emollients, and topical corticosteroids.
- Occupational therapy
To maintain joint function and enhance your way of life, daily tasks can be modified with the help of occupational therapy.
Organ-Specific Management: To address scleroderma consequences and organ involvement, certain medications can be used. For instance, doctors may prescribe drugs to treat gastrointestinal motility problems, control pulmonary hypertension, or enhance lung function.


Treatment Options
To supplement conventional treatment and possibly increase its efficacy, many adjunct therapies and therapeutic choices should be taken into account alongside the normal treatment regimen. Among them are:
Nutritional Supplements:
- Omega-3 fatty acids
Anti-inflammatory properties are exhibited by omega-3 fatty acids, which are present in fish oil supplements. They can lessen inflammation and stiffness in the joints while also enhancing cardiovascular health in general.
- Vitamin D
Immune control and bone health are critically dependent on vitamin D. Owing to limited exposure to the sun and significant gastrointestinal absorption difficulties, those with scleroderma are more likely to experience vitamin D insufficiency.
- Probiotics
Gut and immune system health is supported by probiotics, which are good microorganisms. Scleroderma sufferers may have unbalanced gut flora, according to some research.
- N-Acetylcysteine (NAC)
The body’s powerful antioxidant glutathione is a precursor of NAC, which is an antioxidant. If you are among those who are experiencing scleroderma-related lung damage, you may benefit from it by lowering oxidative stress and enhancing lung function.
Natural and herbal remedies: People with scleroderma frequently turn to natural and herbal medicines as a supplemental or alternative therapy for symptom management and boosting overall wellbeing. The following are several herbal and natural treatments that have been researched for scleroderma:
- Aloe Vera
Scleroderma-related skin complaints like dryness, itching, and tightness have been treated topically with aloe vera gel, which is made using the leaves from the aloe plant. Researchers believe that it possesses anti-inflammatory and hydrating effects.
- Turmeric (Curcuma longa)
The main ingredient in turmeric, curcumin, contains antioxidant and anti-inflammatory properties. Although it can be used in food and as a supplement, turmeric can interfere with some drugs, including blood thinners.
- Chamomile
When applied topically or as a drink, chamomile provides soothing and anti-inflammatory effects. It can also lessen the tension related to scleroderma, ease gastrointestinal symptoms, and encourage relaxation.
- Gotu Kola (Centella asiatica)
In traditional medical procedures, gotu kola is a plant that is frequently used. Anti-inflammatory and antioxidant properties are believed to be the main ingredients in it. It can aid in the healing of wounds and in scleroderma patients’ skin thickness reduction, according to some studies.
- Boswellia (Boswellia serrata)
Ayurvedic medicine has used the anti-inflammatory effects of boswellia for a long time, and is also referred to as Indian frankincense. It is available as a supplement and assists in managing the symptoms of scleroderma connected to inflammation.


Conclusion
Approaching herbal medicines and natural cures should be done with caution. These treatments combined with other medications can have negative effects, and their purity, potency, and dose can vary greatly. Furthermore, because they are not subject to the same regulations as prescription drugs, herbal supplements, and natural remedies can have problems with quality control. To guarantee proper use and prevent any consequences, speaking with a medical expert who is educated about herbal medication is essential.
Additional resources for further reference
https://my.clevelandclinic.org/health/diseases/8979-scleroderma-an-overview
https://www.mayoclinic.org/diseases-conditions/scleroderma/symptoms-causes/syc-20351952
https://www.aad.org/public/diseases/a-z/scleroderma-treatment
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.
Table of Contents


